From VOA Learning English, this is the Health and Lifestyle report.
British researchers say they have grown small human organs using cells removed from fluid that protects developing fetuses.
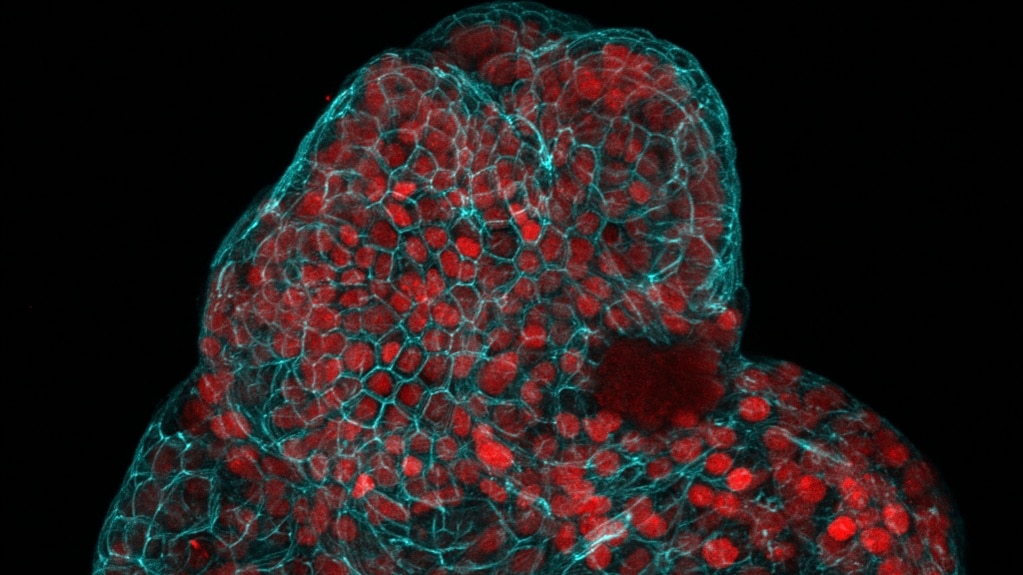
These organs are known as mini-organs, or organoids. They are extremely small, simple structures. They could be used in testing of new medical treatments or to study the workings of full-size organs.
The University College London carried out the study. Researchers collected the cells from fluid removed from 12 pregnant women during routine medical examinations at Great Ormond Street Hospital in London.
The cells then were grown into organoids in a laboratory. The researchers said it was the first time such mini-organs had been produced from cells collected during an active pregnancy.
The scientists said they hope their method will lead to future methods for treating conditions present before birth.
Mattia Gerli of University College London was a lead writer of the study. He told the Associated Press (AP) that he and his team were “really excited” about how their research might result in important new treatment possibilities.
The findings were reported in a study that recently appeared in the publication Nature Medicine.
Scientists have so far produced organoids that look like some human organs, including the brain, kidney, lung, stomach and liver. Lab-grown mini-organs are generally used to study how organs work without the need to experiment on real ones.
The scientists looked for which tissues the stem cells came from and then identified cells from three organs: lungs, kidneys and intestines.
In the past, organoids could only be created from adult stem cells or tissues collected after an abortion. An abortion is a medical operation to end a pregnancy.
The current method does not violate rules that govern direct removal of stem cells from fetal tissue. The amniotic fluid method permits scientists to get cells from fetuses during the latter parts of pregnancy.
Governments around the world have different regulations covering abortions. In Britain, the legal limit for ending a pregnancy is generally 22 weeks after conception. This rule prevents British researchers from studying some parts of normal human development or diseases that are present past 22 weeks.
In the United States, abortion restrictions differ by state. Most states ban the use of fetal tissue for research, said Alta Charo. She is a retired professor of law and bioethics at the University of Wisconsin at Madison. Charo was not part of the latest study.
Fetal tissue is defined by the National Institutes of Health as material coming from a dead human embryo or fetus. The tissue could come from a fetus that was aborted or did not survive because of medical problems with the pregnancy. The use of tissue from an abortion has long been controversial.
Charo said the new method does not raise the same ethical concerns. And taking amniotic fluid during a woman’s pregnancy “does not appear to add any physical risks to either fetus or pregnant woman,” Charo said in an email to the AP.
As part of the experiments, the researchers worked with scientists in Belgium to study the development of babies with a condition called congenital diaphragmatic hernia. This can result in organs such as the liver and intestines getting displaced into the chest. About 30 percent of fetuses with this disease die because the lungs cannot fully develop. If doctors could identify the condition before birth, they could operate on a fetus to fix it.
In the experiments, researchers grew lung organoids from the cells of fetuses with the hernia condition before and after treatment. When comparing those organoids to organoids from healthy fetuses, the team was able to use the lab method to identify the affected child’s condition before birth.
The scientists said this ability to study working, pre-birth mini-organs is the first step toward establishing more detailed prognosis information and improving treatment methods.
And that's the Health and Lifestyle report.
I’m Anna Matteo.
And I'm Bryan Lynn.